GeeseMed, a leading Medical Billing service company provides affordable, accurate, quick, and effective Medical Billing services to healthcare facilities throughout the USA. The revenue cycle management for medical practices has become more complicated than ever. With evolving insurance, company and government policies, as well as compliance regulations and healthcare reforms, it has become difficult for physicians and their staff to keep pace. This results in incorrect or delayed filing of claims and poor reimbursements. Exceptional medical billing services can streamline your revenue cycle to procure better reimbursements, saving you precious time and effort so that you can concentrate on what you do best – patient care.
With our premium medical billing services, collection rates will dramatically increase, as well as your peace of mind. Processing costs are reduced by as much as 60%! We file both electronic claims and paper claims to over 1500 payers across the United States. We have certified medical billing experts at our disposal who focus only on billing (unlike your front office staff, who have to take care of other things in your practice), we bill accurately, dropping the rejected claims rate to 1%-2% and not 20%.
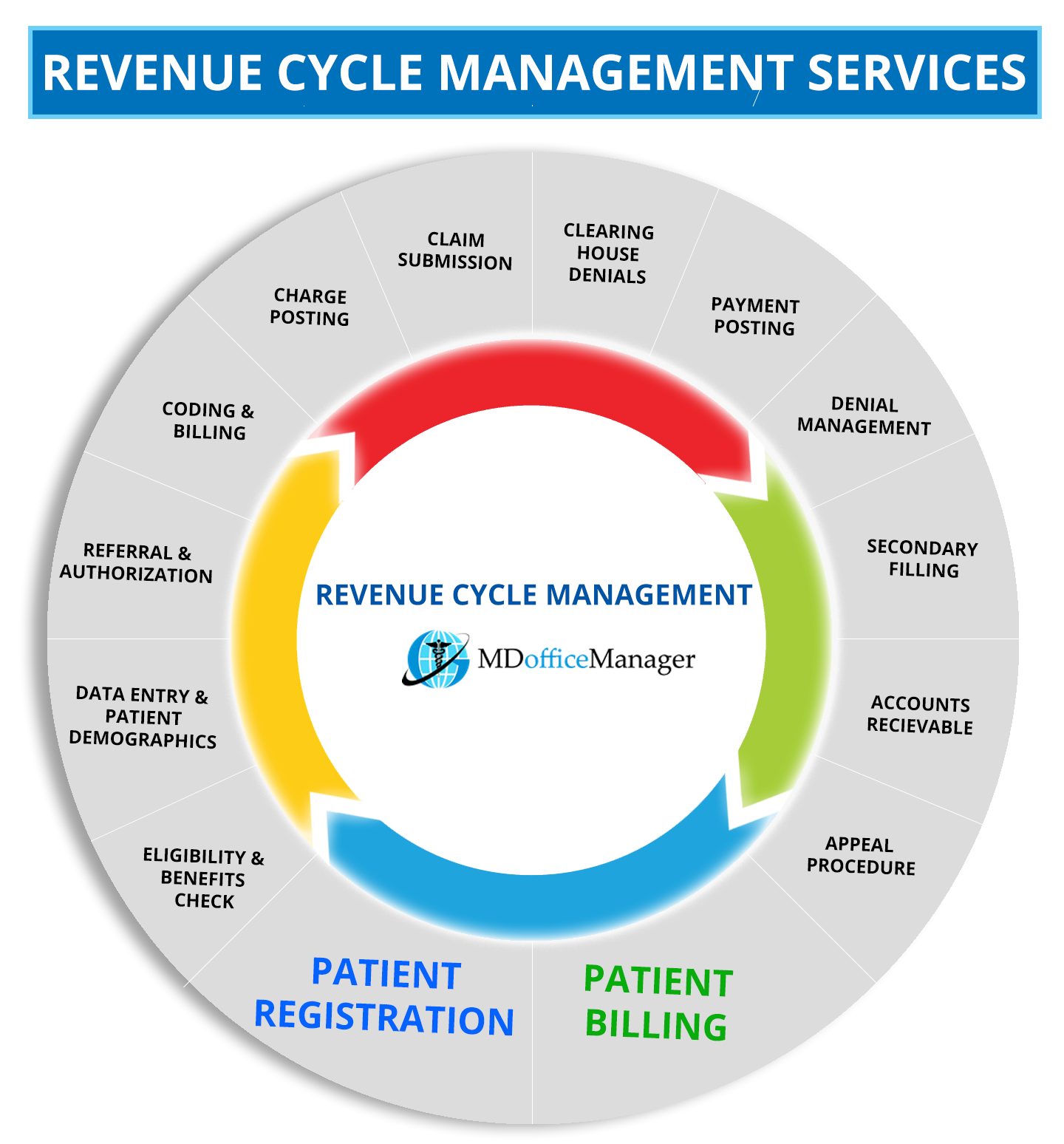
We enter the patient demographic information and verify its accuracy.
We check the benefits and eligibility of the patients before the provider renders service and records it in the Practice Management System.
Coding for diagnosis, services rendered, and appropriate modifiers is verified and set.
Charge information is entered into the system for medical billing claim generation after a thorough reconciliation from both the provider’s office and GeeseMed.

E-claims and paper claims are generated and sent out to payers via a medical billing clearinghouse. Claim receipt acknowledgements are checked and unsent claims are re-filed. Payer responses are checked and processed.
ERAs and EOBs are processed and payments are posted into the system.
Claims denied on EOBs are corrected and re-filed or appropriately appealed.
Monthly billing summaries with collections, billables, and outstanding AR’s will be provided. Client-specific reports are also submitted monthly and/or yearly. You can generate 250+ different reports and see what we do anytime.
We make sure your provider’s record is up to date with all insurance companies.
Mailing there are NO added charges for these services. If you do not require all of the above services we also provide many options for shared services between your practice and GeeseMed.
We provide toll free number to the practice and manage all patient phone calls related to bill, co-pay or deductible amount.
GeeseMed provides reimbursement solutions for healthcare providers. Our revenue cycle management’s knowledge-base encompasses proven methodologies & techniques that leverage continuous process innovation & technology. You will receive 100% transparency, 24/7 reports, and all industry updates such as the ever-changing payer environments, HIPAA compliance, RAC audits etc. In short, GeeseMed is favored among physicians for assisting them with unprecedented control over their finances.
Revenue Cycle Management is a critical part of the financial viability for any health care facility. Our comprehensive medical billing services help to maximize reimbursements, decrease denials, and increase profitability for your practice. Our qualified RCM team files the claims to payers for payment, ensures there is sufficient documentation & appropriately coded by a professional & certified coder, corrects any denied/rejected claims (if applicable), submits the appeal, and reports and documents any claims filing occurrences and trends for continued process improvement.
We provide full-service data entry. All claim information – superbill, patient information, copies of insurance cards – are sent to North American Healthcare Management Services. Our experienced staff will then enter all patient demographic and charge information. This is accomplished by sending the encounter forms to our office. Our billing staff will enter, submit and follow-up on all charges produced by the clinic. Your practice’s or clinic’s banking services can be configured so that payments are sent directly to your bank. The corresponding EOB’s and remittance advice can be sent to North American HMS where they are posted and scanned. You will receive scanned copies as well the original EOB.
A healthcare organization can exert some control over internal dynamics, such as provider productivity, patient volume and fees for services. However, it is more difficult to influence external factors, such as claim reviews by insurance companies, denials and responsible party payment collection. We understand the level of trust that is needed when partnering with an outsourcing company for your comprehensive medical billing. Our experienced and certified staff will provide an exceptional level of service, professionalism and personalized attention to earn your trust and to assist your practice in a seamless approach.
The revenue cycle includes all the administrative & clinical functions that contribute to the capture, management and collection of patient service revenue, according to the Healthcare Financial Management Association (HFMA).
We’re here to help. Send us an email or call us at 812-248-9206 Toll free number 877-786-7604. Please feel free to contact our expert.